In the UK, it is estimated that 3 million people
have COPD, of whom 2 million are undiagnosed. Prevalence increases with
age and most people are not diagnosed until they are in their 50s. There are
significant geographic variations in the prevalence of COPD, and it is
closely associated with levels of deprivation. Unlike many other common chronic
diseases, the prevalence of COPD has not declined in recent years. (from
National Institute for Health and Clinical Excellence (NICE) online)
A special thank you to Dr Joy Gana-Inatimi (MCSP, SRP,
MHCPC, MACPRC, AFHEA): Senior Lecturer at UCLan & Consultant AHP (Chest Medicine
and Pulmonary Rehabilitation), the British lung foundation & NICE.
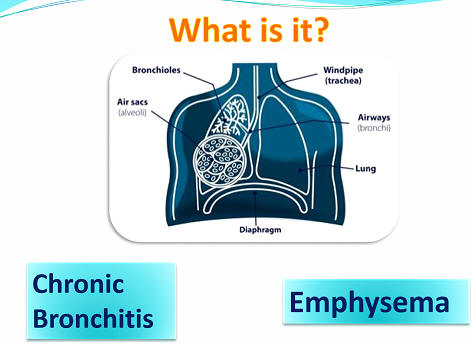
What is COPD? COPD
stands for chronic obstructive pulmonary disease. It is the name used to
describe a number of conditions, including chronic bronchitis and emphysema,
where people have difficulty breathing because of long-term damage to their
lungs.
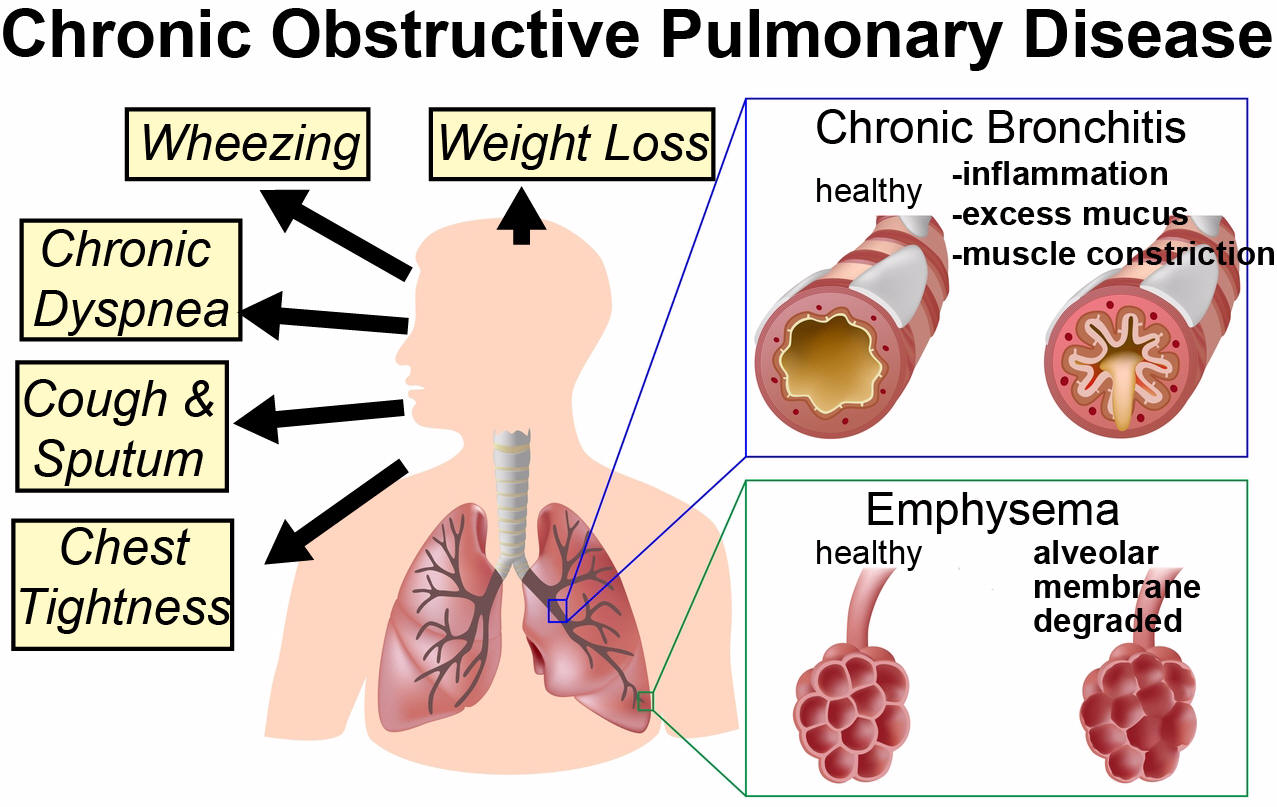
Chronic bronchitis:
Bronchitis means ‘inflammation of the
bronchi’. These are the tubes or airways which carry oxygen from the air to the
lungs. This inflammation increases mucus production in the airways, producing
phlegm which makes you cough.
Emphysema: this is where the
alveoli (air sacs) in the lungs lose their elasticity. This reduces the support
of the airways, causing them to narrow. It also means the lungs are not as good
at getting oxygen into the body, so you may have to breathe harder. This can
result in shortness of breath.
What causes COPD? Smoking,
environmental exposure, fumes/particles at work, it can run in families and
there is rare genetic condition called alpha-1-antitrypsin deficiency makes
people very susceptible to develop COPD at a young age.
How is it diagnosed? There
is no single diagnostic test for COPD. Making a diagnosis relies on clinical
judgement based on a combination of history, physical examination and
confirmation of the presence of airflow obstruction using spirometry (breathing
test).
What are the common symptoms?
Cough, breathlessness, wheeze, phlegm.
How can COPD affect you?
Fatigue, anxiety, weight loss, low mood.
Can it be cured? COPD is
treatable but not curable. Early diagnosis and treatment can help to slow
the decline in lung function and increase the amount of time that people with
COPD have to enjoy an active life. Pharmacological and other therapies can help
to manage symptoms and disability caused by COPD, and improve the person’s
quality of life, despite having only limited or no impact on the airflow
obstruction.
What can you do to help?
There are many ways you can help your COPD.
1. The most helpful thing you can do is to
stop/reduce smoking. If you stop smoking the disease progression is
slowed down. It is never too late to quit and there is a lot of help
available.

Quit
Squad - Lancashire Stop Smoking Service
Email:
quitsquad@lancashirecare.nhs.uk
Website:
www.quitsquad.nhs.uk
2. Attending pulmonary rehab is the second most
effective thing you can do to help improve you lung function. You are
already on your way to helping your COPD symptoms.
3. A good diet will always help your health but
the most important thing to remember is to eat little and often. With
COPD you may find large meals too much to handle but you still require
the same calorie intake.
4. Correct inhaler technique and use of medication
for COPD is essential.
5. You must protect yourself against infections
and therefore preventative measures such as the ‘flu and pneumovax
vaccines are recommended.
6. Knowing how to manage a flare-up (exacerbation)
of COPD is vital.
What is a flare up? Also
known as an exacerbation, a flare up is a worsening of symptoms. For example
becoming more breathless, more wheezy, changes in phlegm (colour/amount),
loss of appetite, reduced energy or poor sleep.
What action should you take during a flare up?
It is important to get medical advice which would
usually be your GP.
Allow extra
time to complete daily activities
Plenty of rest
Relaxation
Controlled
breathing exercises
Huff and puff
to clear phlegm
Eat small
amounts often
Keep hydrated,
lots of clear fluids
When to call 999?
Ø If you are so breathless you cannot
complete a sentence
Ø If you feel drowsy or confused
Ø If there is any chest pain
What are the services available in Preston?
There is a specialist respiratory service based at Royal
Preston hospital, this team includes specialist consultants, nurses and
physiotherapists.
www.lancsteachinghospitals.nhs.uk/respiratory-medicine
There is also the Adult Community Respiratory Service (ACRS),
a team of experienced nurses and physiotherapists who offer a wide variety of
services to patients living with a respiratory condition across Preston,
Chorley, South Ribble, Blackburn and Darwen.
www.lscft.nhs.uk/adult-community-respiratory-central
Nationwide support (video links);
Follow this link to view an inspiring video about how one
lady coped with her diagnosis www.blf.org.uk/support-for-you/copd/world-copd-day
follow this link to hear about living well with COPD
support groups
www.youtube.com/watch?v=vy_Q-HEEjAk
Rachel Imms
Lecturer in Occupational Therapy (UCLan)